Introduction
If you’ve ever experienced sharp, shooting pain traveling from your lower back down to your leg, you’re likely familiar with sciatica. This condition can make even simple daily tasks — sitting, walking, or bending — uncomfortable and frustrating. While pain medication may provide short-term relief, physiotherapy for sciatica plays a crucial role in addressing the underlying causes and helping you return to normal movement safely and confidently.
This article explains how to manage sciatica pain through physiotherapy, the techniques used, what recovery looks like, and why early, targeted care makes a meaningful difference.
Understanding Sciatica
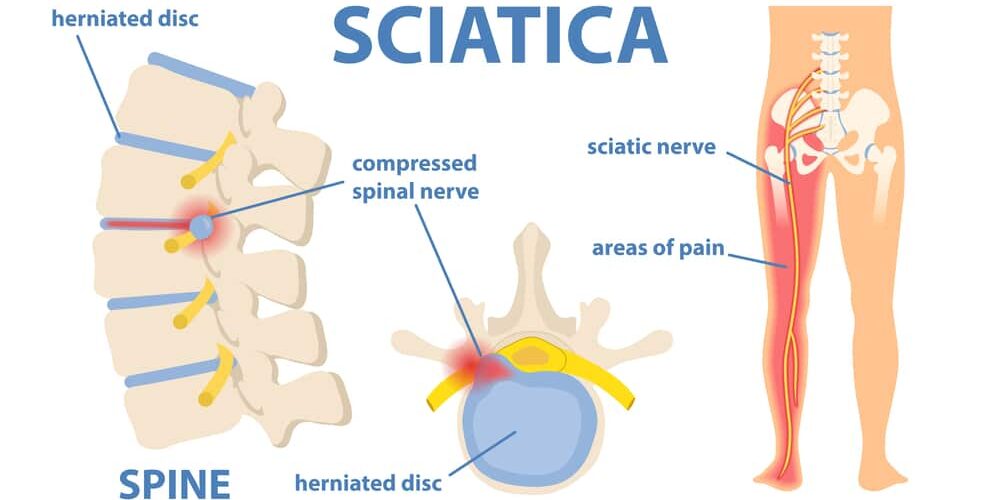
Sciatica refers to irritation or compression of the sciatic nerve — the largest nerve in the body — which runs from the lower spine through the buttocks and down each leg. When this nerve becomes compressed or inflamed, it can lead to:
- Sharp, burning pain radiating down one leg
- Numbness or tingling in the lower limb
- Muscle weakness or difficulty standing and walking
- Increased pain when sitting or bending forward
Common causes include a herniated or bulging disc, spinal stenosis (narrowing of the spinal canal), muscular tightness in the glutes or piriformis, or poor posture and prolonged sitting. This is why sciatica pain treatment must focus not only on the symptoms but also on the underlying mechanical issues.
Why Physiotherapy Is Important for Sciatica
Sciatica physiotherapy addresses both the symptoms and the source of the problem. Instead of masking pain, it aims to restore movement, improve muscle strength, and correct posture — ensuring long-term recovery.
Here’s how physiotherapy makes a difference:
1. Pain Relief and Nerve Desensitisation
One of the first goals of sciatica treatment physiotherapy is reducing nerve irritation. Physiotherapists use manual therapy, gentle mobilisations, dry needling, or soft-tissue release to ease pressure around the affected area. Simple movement-based techniques can also help desensitise the nerve, improving comfort and mobility in the early stages of treatment.
2. Restoring Movement and Flexibility
When pain sets in, the body often compensates by restricting movement, leading to stiffness and imbalance. Physiotherapy works to restore natural spinal and hip mobility through guided exercises, gentle stretches, and posture correction. Improving flexibility around the lower back, glutes, and hips reduces strain on the sciatic nerve and encourages long-term sciatica pain treatment..
3. Strengthening Core and Supporting Muscles
Weak core and gluteal muscles often contribute to sciatica by allowing excess pressure on the lower spine. A structured exercise plan helps strengthen these key stabilising muscles, providing better support for the back and pelvis. Over time, this reduces nerve irritation and enhances spinal stability, making flare-ups less likely.
4. Posture and Ergonomic Training
Prolonged sitting, poor lifting habits, and slouched posture are common triggers for sciatica. Physiotherapists assess your day-to-day movements and teach you how to maintain proper alignment, whether you’re at your desk, driving, or exercising. Adjusting posture and improving ergonomics can dramatically reduce recurring episodes of sciatic pain.
5. Functional Rehabilitation
Once the pain begins to settle, physiotherapy shifts focus to functional movement and real-life activities. Exercises become more dynamic — incorporating lifting, bending, or twisting movements to rebuild coordination and confidence. This stage helps you return to work, sport, or daily activities with confidence, guided by evidence-based sciatica physiotherapy strategies.
6. Long-Term Prevention
Physiotherapy doesn’t stop when the pain disappears. A strong focus is placed on education — understanding your triggers, maintaining mobility, and adopting a consistent exercise routine to prevent future episodes. You’ll also learn simple at-home stretches and strengthening drills that keep the sciatic nerve and lower back healthy over time.
What to Expect During Physiotherapy for Sciatica
Each physiotherapy plan is tailored to your individual needs, but most follow these general stages:
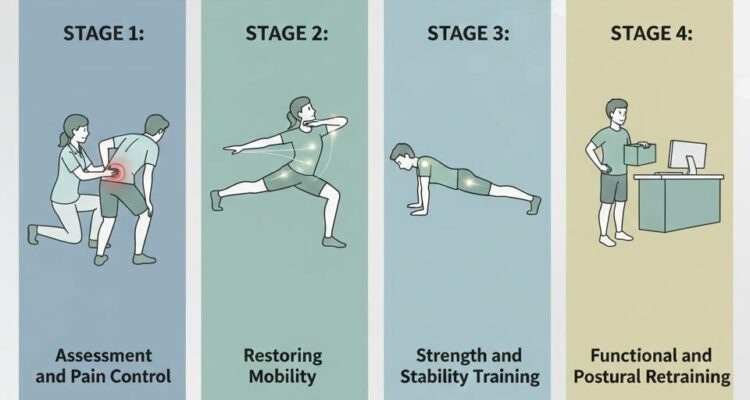
Stage 1: Assessment and Pain Control
Your physiotherapist begins with a detailed assessment of your symptoms, lifestyle, and movement patterns. Initial sciatica physiotherapy focuses on reducing inflammation and easing nerve tension, targeted mobility exercises, and advice on safe movement and rest positions.
Stage 2: Restoring Mobility
As pain decreases, you’ll work on improving flexibility and range of motion in the lower back, hips, and hamstrings. This helps reduce pressure on the sciatic nerve and restore natural movement.
Stage 3: Strength and Stability Training
Next, your therapist introduces strengthening exercises for the core, glutes, and legs to support spinal alignment. This stage is essential for building resilience and preventing future flare-ups.
Stage 4: Functional and Postural Retraining
Finally, you’ll focus on integrating new movement habits into your everyday life. Your therapist will help you refine posture, lifting mechanics, and work ergonomics to ensure long-term comfort and performance.
How Effective Is Physiotherapy for Sciatica?
Physiotherapy is widely recommended as a first-line treatment for sciatica because it addresses both pain relief and movement restoration. Research shows that physiotherapy for sciatica is an effective first-line treatment. It improves pain, function, and mobility faster than passive treatments or prolonged rest. While recovery varies depending on severity and consistency, most people experience meaningful improvements when physiotherapy begins early.
However, the outcome depends on several factors, including the severity of nerve involvement, the underlying cause, and patient commitment to the prescribed exercises. While not every case improves instantly, most people experience significant benefits when physiotherapy is started early and followed consistently.
When to Seek Further Medical Help
While most cases of sciatica improve with conservative care, there are situations that require urgent medical review. You should see a doctor immediately if you experience:
- Loss of strength or sensation in the leg or foot
- Difficulty controlling bladder or bowel movements
- Unrelenting pain that worsens despite therapy
- Pain following trauma or a fall
These may indicate more serious nerve compression that requires specialist assessment.
The Bottom Line
Physiotherapy is one of the most effective ways to manage sciatica because it targets pain, restores movement, and strengthens the body to prevent future flare-ups. With the right combination of hands-on treatment, personalised exercises, and education, you can regain confidence in your movement and return to your daily activities without discomfort.
If you’re experiencing sciatic pain and want expert, evidence-based care, The Movement Mill serving in sydney and surrounding suburbs offers tailored physiotherapy programs designed to help you recover faster and stay pain-free. Book your assessment today and take the first step towards long-term relief and better movement.
FAQs
How effective is physiotherapy for sciatica pain?
Physiotherapy for sciatica is highly effective because it targets the root cause of nerve irritation rather than just masking the pain. Through manual therapy, mobility work, and strengthening exercises, sciatica physiotherapy reduces inflammation, improves movement, and supports long-term recovery. Many people experience significant improvement within a few weeks when they follow their treatment plan consistently.
How long does sciatica take to heal with physiotherapy?
Recovery time varies, but most people start noticing relief within 2–4 weeks of consistent sciatica pain treatment. Mild cases resolve faster, while chronic or severe sciatica may require several months of structured rehabilitation. Early intervention and a personalised physiotherapy plan can help speed up healing and prevent recurring flare-ups.
Can physiotherapy help if my sciatica keeps coming back?
Yes. When sciatica repeatedly returns, it usually indicates weak supporting muscles, poor posture, or restricted mobility. Sciatica treatment physiotherapy helps address these underlying issues by strengthening the core and glutes, restoring spinal mobility, and correcting daily movement patterns. This approach not only relieves pain but also reduces the chances of future flare-ups.
What exercises are best for managing sciatica pain?
The best exercises for how to manage sciatica pain include gentle nerve glides, lower-back mobility exercises, core-strengthening movements, and targeted glute activation. Your physiotherapist will tailor these exercises to your condition while ensuring they don’t aggravate symptoms. These movements help reduce pressure on the sciatic nerve and support long-term recovery.